Abstract
Introduction:
Hematopoietic stem cell transplantation (HSCT) has had a major impact on the treatment of hematologic malignancies. Recent studies have shown the role HSCT can have in gene therapy by providing long-lived genetically modified cells to treat a variety of human diseases. It is well known that HSC and bone marrow-derived cells can differentiate into long-lived tissue macrophages and populate a wide spectrum of tissues including the brain. These cells are termed bone marrow derived macrophages and are akin to microglial cells in both morphology and function. There is an expanding literature of preclinical animal studies focused on the potential benefits of bone marrow derived-macrophage engraftment into the central nervous system (CNS). In this study we report the detection and characterization of donor bone marrow-derived macrophages in the cerebral cortex of allogeneic transplant patients.
Methods:
To determine the frequency of donor cell engraftment in post-transplant patients, we selected a cohort of 20 patients who had undergone a sex-mismatched transplant. Formalin fixed paraffin embedded cerebral cortex samples were obtained from the Fred Hutch tissue repository. Samples from male and female autologous transplants were used as controls. Tissue sections were stained by XY fluorescent in situ hybridization (FISH) to identify male and female cells. The XY FISH-stained slides were imaged at 40X magnification on a TissueFAX system. Scanned images were analyzed in blinded fashion using TissueQuest software. Male donor cells were defined by the presence of the Y chromosome within DAPI stained nuclei. Parameters were established using a small area and then applied to a larger area covering 10,000-15,000 cells. Identified donors were confirmed by manual inspection. Adjacent sections were used in Iba1 immunohistochemistry (IHC) studies to quantify the microglia/macrophage population. Select cases were used in double fluorescent Iba1 IHC (tyramide signal amplification)/XY-FISH studies to identify the donor cell type.
Results:
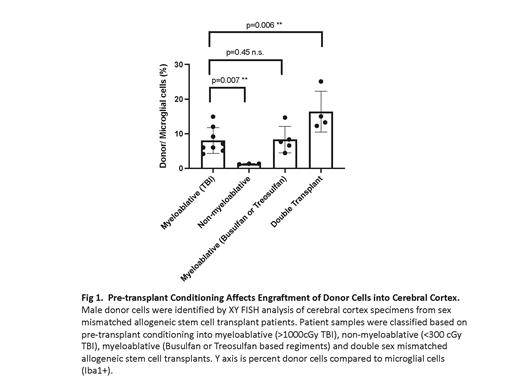
Intraparenchymal donor bone marrow derived cells were identified in all cerebral cortex sex mismatched samples. To determine the identity of donor cells, select cases were stained with fluorescent tyramide based Iba1 IHC, imaged, stained with XY FISH and re-imaged. The majority of donor cells (>80%) showed strong expression of Iba1, confirming them to be bone marrow-derived macrophages. In parallel Iba1 IHC studies we showed that microglial cells constitute ~12% of the scanned cell population. Thus, when computed as a percentage of the macrophage/microglial population, donor cells from myeloablative transplants range from 4.2-25%. The bone marrow derived cells are stable over time since length of the post-transplant period did not have a major impact on the number of donor cells. Prior animal studies have demonstrated the importance of conditioning (total body irradiation (TBI) or Busulfan) in providing access to the CNS and stimulating engraftment. Consistently, we found that the strength of the conditioning regimen had a significant impact on donor cell engraftment into the CNS. Donor cells in myeloablative cases (>1,000cGy) averaged 8.0% (4.2-14.9%) of microglial cells, while those in non-myeloablative cases (<300cGy) averaged 1.3% (1.2-1.3%). In agreement with preclinical studies, we also noted that myeloablative cases from Busulfan or Treosulfan based conditioning had similar levels of donor-derived cells as cases with TBI myeloablative conditioning, averaging 6.6% (4.4-8.3%) of microglial cells. Although only a limited number of samples were available for analysis, the highest level of donor engraftment was observed in patients who had received 2 separate transplants; on average they comprised 16.3% (12.2-25.1%) of microglial cells.
Conclusion:
This, the largest study of bone marrow-derived macrophages in post-transplant patients, shows that donor derived cells from myeloablative transplants account for 4.1-25.1% of microglial cells. Donor engraftment is highest following myeloablative conditioning or in patients receiving multiple transplants, and lowest in non-myeloablative cases. Our studies document the magnitude of donor-derived macrophages in the CNS following a bone marrow transplant and serve as a basis for future gene therapy studies targeting neurodegenerative disorders.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal